June 27, 2019 | A major step forward in making clinical trials less onerous to conduct has been recent sponsor focus on “reducing the amount of paperwork and bureaucracy” put on sites, says Jim Kremidas, executive director of the Association of Clinical Research Professionals (ACRP). Companies have started using shared data platforms, so they already have a lot of the information traditionally asked on site feasibility questionnaires.
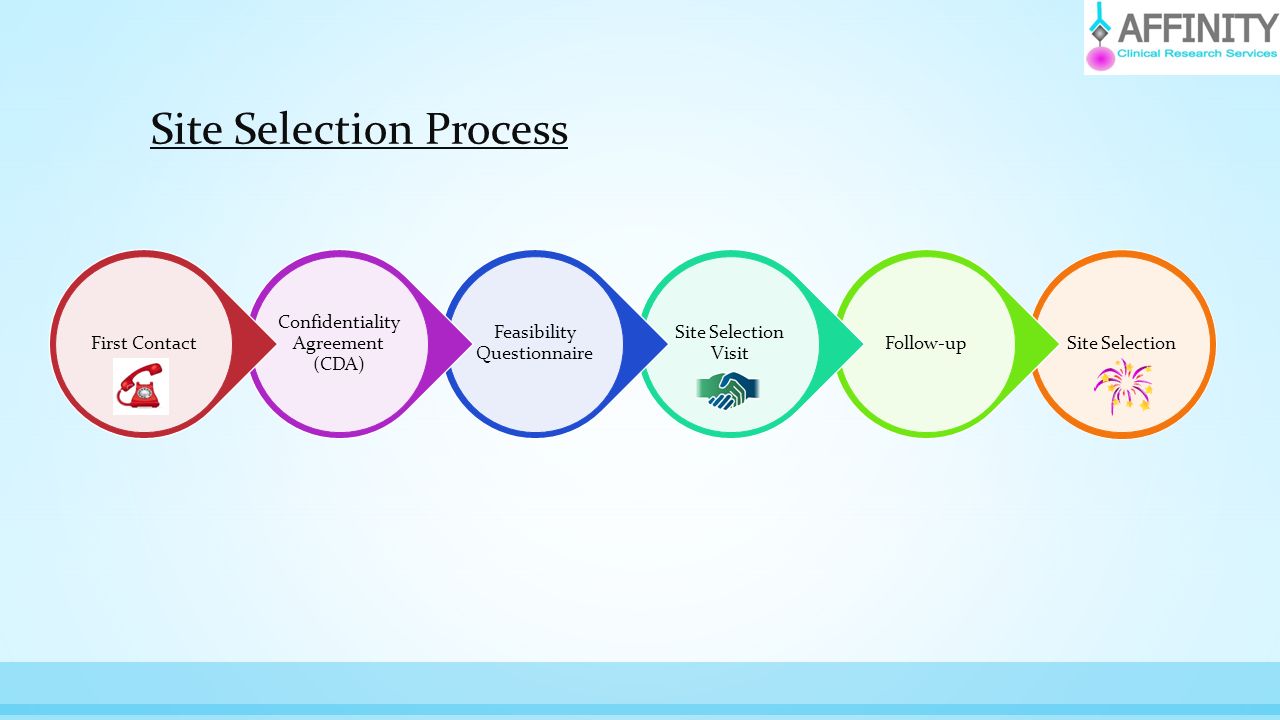
Narrowing the scope of feasibility questionnaires by leveraging data that is available in tools like the TransCelerate Investigator Registry is an emerging industry trend. “As we invest more in technology we are going to be able to get a lot of that information on our own, and then hopefully get to the point—if we continue with site feasibilities at all—where we only send a four- to five-question survey narrowly focused on more unusual study-specific requirements,” says Lorena Gomez, director of global study startup and essential documents at Allergan. “The industry is absolutely heading in that direction… especially companies already using the Shared Investigator Platform [of TransCelerate], where sites are able to maintain facility and investigator profiles that contain much of the information that was historically gathered via feasibility questionnaires.”
Nurse and Patient Panels
Reliance on lengthy site surveys began to wane at AstraZeneca in 2017, coinciding with a new approach to gathering insights to inform protocol design and conduct and enhance the study experience for patients and sites, says Michele Teufel, the company’s patient and site engagement lead in development operations. The company began proactively seeking input from site nurse and patient panels, and study teams started reviewing draft study protocols and patient support materials with nurses. Many of the recommendations made by study teams were adopted—including simplifying the patient consent form, furnishing a patient study visit handbook and website, reimbursing patient travel costs and providing WiFi access at sites.
Building on existing internal and external data sources for feasibility and site identification, AstraZeneca last year piloted the use of real-world data (RWD) in a federated electronic health record (EHR) platform to identify potential patients and study sites, says Sandra Smyth, director of the company’s global feasibility and recruitment group. The RWD comprises more than 75 million live EHRs from more than 100 hospitals in 20 countries via licensing agreements with InSite and TriNetX. For some EHR-identified sites, feasibility surveys became “smarter and simpler,” focusing on areas where reliable information or data was unavailable, she adds.
The study team for a recent pediatric study used EHR platform to find five new suitable and interested sites with 250 potential eligible patients within two weeks, Teufel adds. “These sites are in progress for start-up.”
AstraZeneca is now developing a new digital data-driven feasibility and site identification tool, known internally as Merlin, to integrate multiple data sources onto one platform, says Smyth. Its introduction is part of a transformation program it calls “Our future reimagined” that aims to “optimize the use of data, speeding up the delivery of medicines to patients and freeing up scientists’ time for innovation.”
Merlin’s data sources currently include the company’s internal clinical trial management system, IxRS, Citeline, and ClinicalTrials.gov, says Smyth. The list will “continuously expand” to including RWD (e.g., claims and EHR) and data related to prevalence and incidence, publications and drugs. “There will be ongoing curation of data and the ability to apply predictive modelling,” she adds.
Smyth describes key features of the new platform as follows:
- Single, global optimized site and investigator list that meets quality thresholds and study constraints
- Optimal scenarios predicting activation, recruitment speed, and cost
- Early indication and landscape feasibility to quickly pinpoint potential countries
- Predicted randomization rates and reference studies
- Automated workflow to incorporate local country intelligence to use in balance with data
In addition to reducing the manual effort in merging disparate data sources and data analysis, Smyth says, Merlin’s expected benefits also include greater focus on strategic feasibility planning at the program level less time spent coordinating feasibility surveys across high-volume sites at the study level. More informed, data driven decision-making will be balanced with real-time targeted site and patient survey, and local validation of sites, by final protocol—all of which translates into increased data integrity and speed in bringing potential new medicines to patients.
AstraZeneca is partnering with an external vendor for the initial build of the platform, Smyth says, and first features should be implemented by the end of 2019.
Certification Matters
As has been recently uncovered, how “professionalized” sites are matters a great deal when it comes to choosing investigators, says Kremidas. An analysis by WCG found that study coordinators who were ACRP-certified did significantly better at enrolling patients and had far fewer protocol deviations. Principal investigators who were ACRP-certified similarly perform better.
Study results were presented last June at DIA 2018, says Kremidas, and are starting to get the attention of sponsors and CROs. “The study coordinator in particular is absolutely critical to the success of a trial… sites with ACRP-certified coordinators, generally speaking, perform in the top quartile.”
Kremidas hypothesizes that where investigators are certified, study coordinators are as well because “the site supports that mindset of professionalizing the role.” A study a few years back found that sites with certified coordinators did better than those without them, as did sites with certified rather than non-certified investigators, but sites that had both saw a statistically significant difference in performance. “Consider the coordinators air traffic controllers,” he says. “You want those people to be professional and you want them to have qualifications.”
The ACRP certification process is evolving to stay in step with changing roles in clinical research, Kremidas says, as reflected in the recent additions of a category for “certified professional” and a new subspecialty designation specific to project management. Soon to be added is a new certification for “medical device clinical development,” he adds.
Less than 10% of all investigators and coordinators are currently certified, “which is a shame,” Kremidas says. All other types of healthcare interaction—even a manicure and haircut—involve licensed professionals. “But there are literally no qualification requirements for clinical study coordinators, zero, nothing. It’s scary.”
Hopeful Signs
One important development, beyond improvements to the site feasibility process, is “clinical research as a care option”—a concept being formally explored by healthcare institutions around the country, says Kremidas. The idea is to expedite referrals from primary care physicians to specialists conducting studies appropriate to the condition and needs of patients. Several new-to-market organizations, including Javara and Elligo Health Research, are trying to help institutions expand access to trials in this way. “It could revolutionize the industry quite significantly.”
Many people don’t have access to adequate healthcare, notes Gomez, and as clinical research has become “demystified” over the years, more of those patients have been getting referred to a trial as a care option. Recruitment into studies should also improve if more sponsors identify trial sites based on where patients are already going for care.
“If a site has loads of patients but is not engaged in clinical research, there are now several vendors that can help to place a coordinator there,” Gomez says. Some companies have successfully used this tactic to build a rapport with research-naïve investigators and gain access to an untapped pool of patients.
IQVIA has a vast ecosystem of data streams to tap when looking for new sites, says Allen Kindman, IQVIA’s vice president of clinical planning and analytics. Sometimes it’s a registry that provides “an unusual insight about what’s going on at an institution or with a disease,” and in other cases consumer data that might “help mold how we do site selection,” including how sites and geographies get preferentially ranked.
While all sites like to think of themselves as high performers—the so-called “Lake Wobegon effect”—some investigators truly don’t need any help, says Kindman. They “enroll far more than anyone else and their quality is far higher. They’re just well set up and highly motivated.”
The data, algorithms and methodologies IQVIA is putting in place can “turbocharge” even the great performers, says Kindman. But he expects the greatest impact to be on the performance of investigators who “should be hitting their targets and just don’t.”
The view of Laura Galuchie, director of global clinical trial operations at Merck, is “no single approach is going to work for every company.” Feedback from multiple sources is required to find the best fit between protocol and site, she says, “which at the end of the day is a win-win-win for everyone involved—sponsor, sites and patients.”
